Waiting For The Doctor At The Foothills Of Bhutan And Arunachal

The mesmerising terrains of Udalguri attract everyone to breathe afresh. People come there for its enthralling wilderness, stay for sometimes and then leave; but the locals of Udalguri have to carry on the struggles every day, whether for their livelihoods or against diseases. Travelling through the length and breadth of Udalguri provides one unique experience of unalike landscapes, the heterogeneous demography and cultures, wide variety of livelihood means. The district in the BTR (Bodoland Territorial Region) shares an international border with Bhutan and with another north-eastern state of Arunachal Pradesh at its north.
But when one looks at the health care facilities available in such a beautiful place, it opens up multifarious concerns that need to be pondered upon, especially at the time of a pandemic. The district has a good network of government health infrastructure in various forms. However, the manpower available at these health structures can surprise anyone to find that even a pandemic could not awake the government to revamp the system which actually was needed. In fact, the district’s health infra anyways needs a major upgrade in terms of doctors, nurses and other staff.
The census data of 2011 says that the district had a population of about 8.32 lakhs and in contrast, when we look at the strength of doctors in Udalguri having such a population, the district administration website will provide us with a number that appears to be not-so-impressive. Moreover, the list of doctors as per the district administration website includes homoeopathic, ayurvedic, general MBBS and those who are deployed under the compulsory rural posting scheme right after completion of MBBS. Interestingly, this list includes a meagre number of specialists. This itself reveals the status of the government health care facilities.
Dr Ganesh Das was a busy man in the Udalguri Civil Hospital (district hospital) on the day we visited the premises. Dr Das is an orthopaedic specialist and during the hours of the OPD (Out Patient Department), he had to check numerous cases fractures, soft tissue injuries, accident cases. While we were sitting inside his cabin patents that were supposed to visit another department or doctor also peeped into it. They literally did not know who to approach for their diseases. “The rural people still are in dark about even the most common medical terminologies. I had experiences dealing with people who needed intervention in pulmonary complications and patients with gynaecological problems as well. We doctors need to guide the people on who should be approached for their complications.” When asked why there is a massive lack of awareness and why not the health department has taken the pains of raising awareness, he simply smiled.
Dr Das provided some of the basic information about the district hospital. Although it is a 200 bedded civil hospital, in practicality the hospital has a functioning capacity of 100 beds, according to Dr Das. He added— “This is a 24X7 hospital and at night there is a doctor in the emergency (casualty) ward. We are about 16 doctors here and have to divide our routines into emergency and OPDs. But the hospital has a sufficient number of nurses.” The civil hospital has to cater for a population of 8-9 lakhs. The civil hospital or district hospital is the highest form of government health facilities in a district, under which BPHC (Block Public Health Centres), CHCs (Community Health Centers), State Dispensaries and Health Sub Centers function with each of these catering to variable population size. Udalguri has three BPHCs, according to Dr Das.
Dr Das also mentioned the prevalent diseases and health problems in the locality— “The peak season of infections start from April/May up till July/ August every year. The majority of the diseases are fevers of unknown origins, Typhoid, Malaria.” Interestingly, he mentioned the high prevalence of RTA (Road Traffic Accident) that doctors have to deal with here. It is not only him, most of the hospitals we visited told about RTA, which appear to be high in the district. Along with it other cases of injuries like falling from trees that cause soft tissue damage are also high in numbers.
Notably, Udalguri has been amongst the high prevalent malaria districts in Assam; in every health facility, one finds the malaria testing kit readily available. Dr Das told that in the year 2009-10 there were massive outbreaks of the disease. Lately, malaria has been controlled to a great extent here.
In the civil hospital itself Dr Bhagirath Dey, MD Medicine and SMO (Senior Medical Officer) had been the Covid nodal officer as well. Dr Dey spoke to NewsClick describing the pandemic response. “During the first wave, the hospital had a facility of 90 general beds along with 5 having semi ICU facility. Labour rooms were functional separately and there had been cases of deliveries from Covid patients as well”—Dr Dey said. “But whenever there was an overflow of patients we had to refer them to either the CCC (Covid care centres) in mild and asymptomatic cases and to Tezpur Medical College & Hospital at Tumuki or to Gauhati Medical College and Hospital.” The CCCs are makeshift health care centres dedicated to Covid patients and they were set up in many premises including that of schools and colleges. Notably, Guwahati is over 100 kilometers from Udalguri Civil Hospital and Tumuki is around 60 kilometres away. Dr Dey said that the hospital has one ambulance and during the peak of the waves the 108 ambulance facilities were functional and were used for transferring serious patients.

The Covid Isolation Ward in Udalguri Civil Hospital.
“During the second wave, there were 35 general beds and 5 semi ICU beds for treating Covid patients. And during this time, we needed oxygens that did not suffer any major scarcity. We used to fill them in Tezpur and Guwahati. There were 18 deaths, most due to comorbidity in the hospital”—Dr Dey added further. Regarding the testing tracing and isolating, Dr Dey said that random testing was also conducted in the villages with the help of the ASHA (Accredited Social Health Activists) along with regular testing in the hospital. The ASHA workers were extremely helpful and took extra pains during those periods, he said.
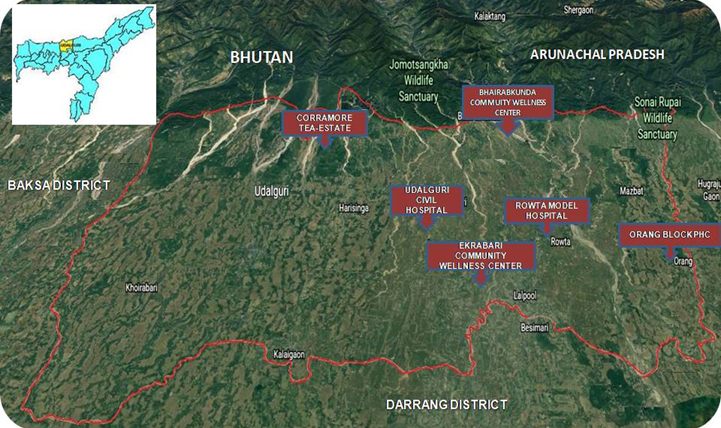
The map shows the points visited by NewsClick during the research.
Going a bit further westward from the Civil Hospital NewsClick reached the Harisinga Model Hospital. Set up in a rural area this model hospital was established during the early period of the pandemic, on February 16, 2019. At that time, people there were completely in dark about a pandemic going the ravage through the world. Reaching there at noon, we found the hospital wearing a deserted look. However, the doctor and some nurses were inside it.
Dr BK Daimary, the deputy superintendent of the model hospital spoke to NewsClick and the anxiety of lack of facilities were quite obvious in his words. “The model hospital is 30 bedded, but we have only 2 regular doctors here along with one posted under compulsory rural service scheme and 10 GNM (General Nursing and Midwifery) nurses”—he said. The model hospital has 6 sub-centres under it and it has to cater for a population of about 1 lakh.
Dr Daimary said that during the Covid peak time there had been oxygen scarcity in the hospital, however, doctors from the district hospital used to come in here when necessary. The only option that the model hospital was left with was to refer the patients to the nearby CCC in case of mild symptoms and the serious ones to the Civil Hospital or to Tumuki (Tezpur Medical College & Hospital).

The Harisinga Model Hospital, Udalguri.
“There are 5 posts of doctors in the model hospital but 3 of them have been attached with the civil hospital and they provide their service there. The rest two have not joined as of now”—Dr Daimary said. The problem with the attachments of posts is that in the record the model hospital has 5 posts and so they have no scope of complaining about a shortage of doctors. But in reality, the service is not provided here and the model hospital remains as such. Dr Daimary expressed his griefs in the continuation of such a scenario even amidst a pandemic and when further surges are anticipated due to Omicron.
Testing, tracking and vaccinating in the nearby areas were also very difficult, according to Daimary. The rural people had huge hesitancy for taking the vaccines and they fear testing positive due to which the people who had fevers simply avoided coming over to the hospital. Vaccine hesitancy however has waned and the situation is better now, Dr Daimary said. The resistance of people in getting tested and accepting the vaccine could be visible in all over Udalguri.
From Harisinga, we went to one of the extreme northern parts of Udalguri, in the Corramore Tea Estate. The rugged roads lead one to inside the estate. One of the big tea estates of Assam, Corramore is owned by the Williamson Magor group. It sprawls in an area of about 488 hectares and spreads close to Bhutan hills. In this way, this area also shares an international border.
Dr Nabajit Hatibaruah, the SMO (Senior Medical Officer) is the doctor who is appointed in the hospital inside the tea estate. This hospital is managed by the tea company, in fact, every tea estate has such a hospital meant for the employees and the workers. However, the hospital has only one doctor in the form of Nabajit Hatibarua, which is the case in most tea estate hospitals. According to Dr Hatibaruah, the tea estate has more than 5000 workers and employees and a single hospital is grossly insufficient. The Corramore hospital is a 45 bedded hospital according to him.
Dr Hatibaruah expressed extreme difficulties in testing, tracing and vaccinating the tea workers. He said— “They are extremely resistant and nobody can convince them. During the second wave, we detected 69 covid positive cases, but the family members of the asymptomatic will come and charge us of some conspiracy. They will say—if the person is not showing any symptoms how can he be positive?” Dr Hatibaruah also said that they had to stop testing at some points. The same was the case with vaccination drives. “Believe me, there were around 50 rounds of vaccination drives inside the tea estate.” However, there were no serious patients inside the tea estate according to him. But, Dr Hatibaruah’s words could easily give the impression that there was no special drive from the government inside Corramore, apart from providing the vaccines and the vaccinating teams.
The tea workers, who live at extremely low wages (205 per day) have their daily struggles to concentrate more than the disease, a few of the workers that we met said. Interestingly, all of them chose to remain anonymous.
From Corramore, we moved to another extreme north point of the district, Bhairabkunda. The Bharaibkunda is an important tourist spot and it also shares an international border with Bhutan and adjacently with Arunachal Pradesh. In that sense, the tiny health centre right beside the tourist spot, the Bhairabkunda HWC (Health and Wellness Center) is not only the last such health facility of Assam but also of India.

The Bhairabkunda HWC, at the border of Assam and India as well.
The HWCs were previously sub-centres. “The difference the HWCs have with a sub-centre is that it has a delivery facility”—said Bidisha Das, the CHO (Community Health Officer) in the Bhairabkunda HWC. The HWC has no doctors as such but has 2 ANMs (Auxiliary Nursing Midwifery). “We have to cater a population of 5,356 in 7 villages”—Bidisha Das told NewsClick. The HWC can provide antenatal care and they follow routine vaccinations. Bidisha also told us that there had been a Covid vaccination drive as well. The HWC also carried covid vaccination drives, said one of the ANMs presents that day along with efforts of random testing in the villages. The HWCs only provide basic medical services, they are not equipped with any facilities other than it.
Pranay Narzari, one of the SW (Surveillance Health) workers present there told us something interesting. He was reminiscing the fear of Malaria in the area. “During last year we did not have any malaria case”—he told. To control malaria, Narzary told, there had been wide-scale campaigns and efforts like providing free mosquito nets, spraying of DDT in the villages. “Some research team used to come and collect the malaria mosquitoes and they took it with them, we don’t know what did they do with the mosquitoes”—he said us laughing.
We visited other such HWCs as well. One such is the Ekrabari HWC, at the southwest part of Udalguri. Payel Banik, the CHO there expressed her anxiety over not having a single nurse in here. Payel said—“I and the pharmacist at the HWC have to handle the patients daily. On average we have above 30/40 patients which increase during the peak season.”

The Ekrabari HWC.
The Ekrabari HWC has to cater for a population of 10 thousand, according to Payel. The area has a mixed population structure, comprising Muslims, Bodos and others. Payel said vaccine response is better among the minority population, which was carried out by the HWC with help from the Civil Hospital.
In a situation like the pandemic, a health structure like the HWC, which stands at the base of the health care hierarchy, can be the most insignificant one. Forget about ICUs, even for emergency cases during the night, there will be no basic services. Moreover, places like Ekrabari is not easily reachable, even an ambulance will take some time to reach there.
At the time we reached Ekrabari HWC, the CHO from another nearby HWC, was also present there. Mr Khyam Newar is the CHO of the Aminpara HWC. He told that his centre has to cater for a population of over 7000 people, however, there is an ANM nurse in the facility.
On the extreme southeast of the district is the Orang CHC (Community Health Center). Dr Binita Sarma, SMO there told us that the CHC is also combined with the BPHC (Block PHC). “Both the CHC and the Orang BPHC are running from the same premise”—she told us.

The Orang CHC
At around 2 PM, the hospital with reasonably good buildings had only one doctor. Dr Binita expressed her anxiety about the heavy shortage of doctors there. She said that only two full-time doctors are there with around 10 nurses. “We few people are running this hospital”—Dr Binita told.
She said that most of the time they have to deal with RTA (Road Traffic Accidents) and other injuries. The Orang CHC has widely expanded tea garden areas (Like the Mazbaat tea garden, Prang tea estate etc.) near its vicinity along with Muslim populations nearby. Dr Binita told that they have to deal with many cases referred to here by the tea garden hospitals (like the one we discussed Corramore). The Orang CHC has only one ambulance and is functional 24X7. “We stay in the quarters inside the campus and have to rush whenever there is an accident case, either at day or at night”—She told. We could not meet any other doctors there who could have told us about the measures taken during the covid peak times. Dr Binita, as she told us, was not much into Covid duties. But, the lack of doctors and other manpower in a big CHC can really shock one.
Fatema Khatun, a resident of Jangalpara villages nearby, who came here to treat her fracture told us— “There are no x-ray facilities in the hospitals, we do it in private facilities. And in serious cases, we have to go to Tumuki.”
Coming from Orang we visited the Rowta Model Hospital established in 2016. A doctor that was present there at the time of our visit, who chose to remain anonymous told us that the model hospital has the highest delivery cases in the entire district. However, there are very few facilities to admit to the hospital. It has only one ambulance, which is not functioning yet.
The anonymous doctor told us the lack of facilities provided during the Covid peak times as well. “PPE kits were unavailable for around 3 months during the second wave”—he said. The hospital has no capacity for X-ray and sonography, forget about scanning. “Random testing was conducted to meet with the target given by the district administration. The positive patients were referred to the CCCs, Tumuki or the Civil Hospital”—he said. The model hospital has to cater to around 35,000 people in more than 5 villages. The doctor also reverberated what Dr Narzary of the Harisinga model hospital shared with us— “doctors are posted here but attached with the civil hospital and they provide their services there”—the anonymous doctor told “even I have to go the civil hospitals three days a week. People get transferred here but they want to stay in towns and get their posts attached to either the civil hospital or other hospitals in the town areas.”
Udalguri district despite having extended infrastructure seriously lacks manpower. The residents of the districts who we talked to also expressed the same concern. Bikram Basumatary, a youth from the Gerua village told— “We actually need more and more doctors. In the civil hospital as well a dental surgeon may treat a patient having fever or other diseases. The public is unaware, but the health system also does not take any steps to improve the situation. The doctors perform their duties hurriedly in the government hospitals, but when they go to private facilities their behaviour improves. Moreover, the doctors prescribe the medicines promoted by the MRs (medical representatives). They should prescribe those medicines available in the hospitals. The supply of medicine is also not adequate.”
“There are other issues as well. X-rays are done in some hospitals, but there are no doctors who can check them and give the impression. The X-ray films are sent to specialists and they interpret online. For ultrasound, one needs to take dates and sometimes it becomes a very lengthy process.”
The reporter’s research was supported by a grant from Thakur Family Foundation. Thakur Family Foundation has not exercised any editorial control over the contents of this research.
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.
























