COVID-19: The Coronavirus can Also Infect Immune Cells
Our defence mechanism works round the clock and, without any notice, and protects us incessantly from pathogens or infection-causing agents. The defence mechanism, called the immune system, provides its service through various cells and molecules. The cells of the immune system are of various types, and they orchestrate the multifarious activities needed for wiping out the attacks of pathogens.
The COVID-19 pandemic, which is still far from over, has opened up many aspects of the functions of the immune system with many new and interesting findings. The new findings can be bundled up for further research and can appear as a knowledge repository for future outbreaks or even pandemics. One of the hallmarks of COVID-19 is an overreactive immune system which causes severe disease and even death.
Exploring the basis of such hyper immunity and the remedies have strengthened our knowledge, with newer information pouring in regularly. In such an endeavour, two research studies recently pointed out that SARS-CoV-2, the coronavirus that causes COVID-19, can even infect the immune cells, the cells dedicated to wiping the pathogen. This kind of infection concomitantly results in more inflammation and disease severity. One has been published in Nature, and the other one in the preprint server biorxiv.
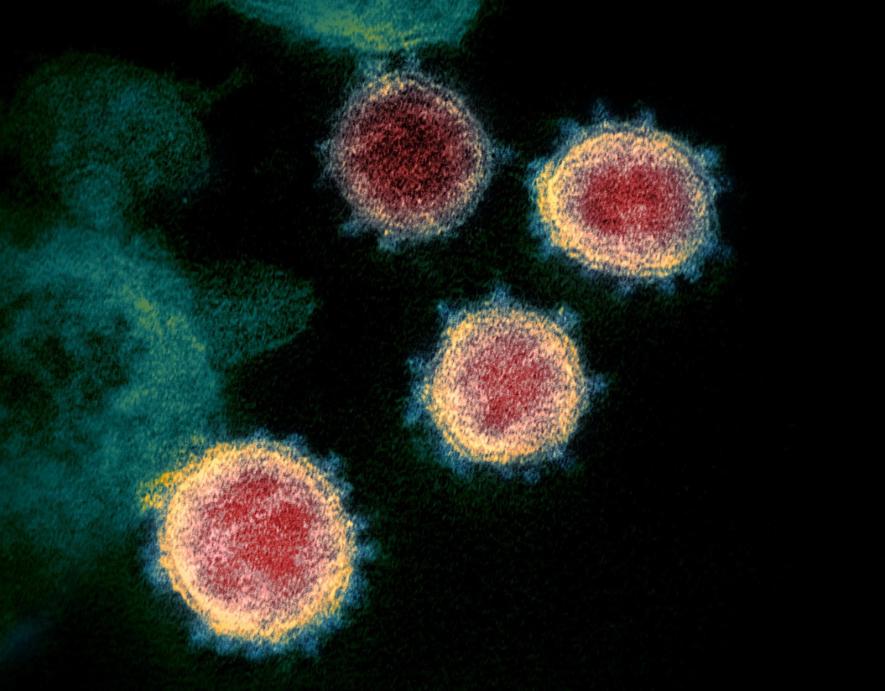
The Nature paper, led by immunologist Judy Lieberman at the Boston Children's Hospital, USA and her colleagues, analysed blood samples collected from COVID-19 patients. The team of researchers looked for monocytes, a type of immune cell. They found that only 6% of the monocytes underwent a type of cell death known as pyroptosis. Pyroptosis is associated with inflammation. Notably, monocytes are the immune system's early responder cells and patrol the body for invading pathogens. When the researchers looked into the dying cells, they found that they were infected with the coronavirus. They suggest that the virus activated the inflammasomes. Inflammasomes are large molecules that can trigger a cascade of responses leading to inflammation and cell death. The researchers found that a quarter of the macrophages activated inflammasomes, and a fraction of them got infected by the coronavirus.
The researchers also looked at another type of immune cell known as macrophage in the lungs of COVID-19 patients who succumbed to the disease. The macrophages are the immune system cells that collect cellular debris, including viral debris. It was difficult to show whether the macrophages were infected by SARS-CoV-2 or collecting the debris.
The other study in biorxiv, led by immunologist Esen Sefik at Yale University, USA, found results aligned with Nature's paper. The researchers found that the coronavirus can infect macrophages in the human lungs and replicate them. The macrophages showed similar inflammatory responses as in the Nature study and eventually died. The team also conducted their experiment on a mouse model.
The Yale team also found that drugs provided to the mice that blocked inflammasomes could prevent the severity of respiratory distress. The inflammasome blocking drugs could rescue mice from developing severe diseases.
There were also some startling findings in the study. Richard Flavell, an immunologist at Yale and also Howard Hughes Medical Institute and a co-author of the study, said—"The macrophages' inflammatory response could be their way of stopping SARS-CoV-2 from replicating. When inflammasomes were activated, the virus stopped replicating in the cells. But when the inflammasomes were blocked, the macrophages started producing infectious virus particles."
This can be crucial as far as immunity against the coronavirus is concerned because the cells dedicated to protecting (macrophages) can get infected themselves and assist in developing disease severity.
However, some other experts comment that further follow-up studies are needed before coming to a concrete solution.
Both the studies also looked into viral entry into human cells and found that the coronavirus can enter immune cells. However, there is a jolt, as the immune cells generally lack ACE2 receptors on their surface. Worth recalling here is that the ACE2 protein found on the surface of cells is the starting point of entering the virus into human cells. The spike protein of the virus clings to ACE2 and, by undergoing a complicated process, makes entry into the human cell.
The virus plays a trick while entering the immune cells lacking ACE2 protein. It utilises antibodies (protein molecules produced by the immune system) that are meant for killing it to enter into a human cell. With the help of antibodies, the virus sneaks in via a different protein present on the cell surface, known as the Fcy receptor. The virus encounters the antibodies attached to the Fcy receptors, and instead of getting disabled, they get entered into the cells.
However, the researchers said that not all antibodies help the virus enter our cells via the Fcy receptor. The Nature paper suggests that people vaccinated with Pfizer and BioNTech jab did not allow immune cells to take up the virus.
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.