Wealth and Social Inequalities Correspond to Health Status of Groups: Report
There are sharp inequalities in terms of various health indicators that exist across different caste, religious, class and gender categories, according to a recent report by Oxfam India. The findings show that the health status of a group of people is contingent upon their socioeconomic position and the poor and the marginalised groups are the worst sufferers.
“The trends of various health indicators across the socio-economic groups that the report has studied indicates that despite a considerable reduction in the gap between the privileged and the marginalised, inequality persists,” said the report titled “India Inequality Report 2021: India’s Unequal Healthcare Story”.
Oxfam released the study on Monday, July 19. The findings of the report are primarily based on secondary analysis of the third and fourth rounds of the National Family Health Survey (NFHS) and various rounds of the National Sample Survey.
Staying-at-home and social distancing have been additionally promoted by the government along with other safety measures such as wearing of masks and frequent hand-washing to curb the spread of the virus. However, according to the report, maintaining social distance and other sanitary prescriptions become extremely difficult to follow for people who live in cramped spaces and use community toilets. The average household size in India is 4.4514 and 59.6% of India’s population lives in a room or less, according to the report. This means that the poor and the marginalised have been finding it much harder to follow protocols, as most of them have precarious living conditions.
“It has been easier for the rich and even the middle class to stay at home and follow safety protocols simply because of access to more space,” the report said.
As the pandemic started spreading, most health systems prioritised services related only to COVID-19. Human and material resources like hospitals, beds and intensive care units were diverted towards the management and treatment of COVID-19 patients. Health services catering to non-Covid illnesses were halted, leading to unprecedented hardships and sufferings for chronic patients and those requiring immediate medical intervention such as pregnant women.
The report said, “The immunisation drive was also disrupted. India vaccinates around 20 million children every year and its disruption might add to the largest number of unimmunised children in the world.” According to the data presented in the report, the was a huge difference in child immunisation rates between the Hindu and the Muslim Populations. For Hindus, the immunisation rate was 63% , while for Muslims, it was only 55.4%. There were also large discrepancies when the immunisation was categorised by wealth. For those with low wealth, the rate was 52.8%, it was 64.2% for those with medium wealth, and a much larger 70% for those with high wealth.
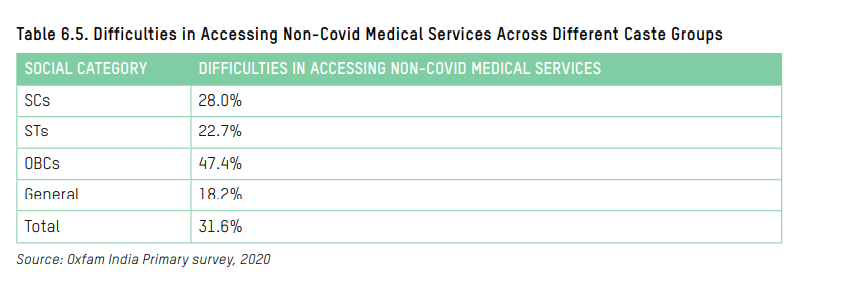
There is also a rural, urban divide. Accessibility to non-Covid medical services was grimmer for patients in rural and hard-to-reach areas as compared to urban areas due to the unavailability of health centres in the vicinity and the lack of transportation facilities.
A similar trend of inequality was seen for Infant Mortality Rate (IMR) across the country. The IMR among the poorest section of the population was very high, at 56.3 (per 1,000 live births), while for the richest section it was 19.8. The majority of the stunted children belong to the rural areas, and are from the poorest section of the society. Stunting was highest among children belonging to the ST category. The stunting rate for ST children was 43.8%, while for the total population of the country it was much lower at 38.4%. The proportion of wasted children was also the largest for the ST category, with a child wasting rate of 27.4% as compared to 21% for the total population.
Similarly, anaemia in children was higher in rural areas (59.5%) than urban (56%), higher for Muslims (59.5%) as compared to Hindus (58.7%), higher for the poorest (64%) than the richest (51.8%), and yet again, at 63.3%, worst for the ST category as compared to 58.5% for the total population.
Disruptions in the availability of drugs for non-communicable diseases (NCD), tuberculosis (TB), contraceptive and other essential services were also reported. Telemedicine—the practice of caring for patients remotely—for which guidelines were issued by the Government of India in March 2020 to facilitate access to medical advice made consultations easier for one section of the society. However, for those with no smartphones and internet connectivity, particularly in rural and hard-to-reach areas, seeking medical advice remained a difficult task.
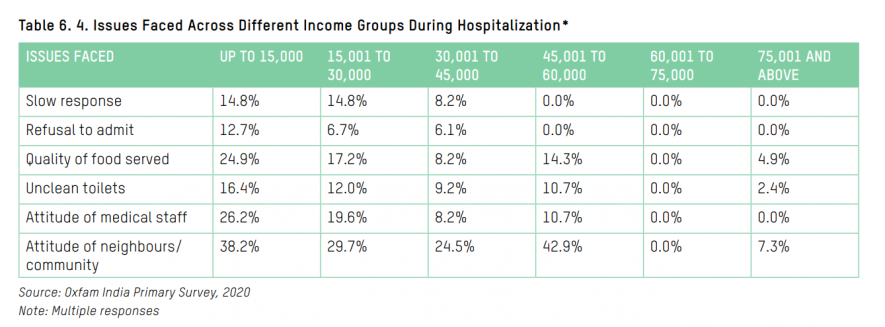
Over 38% of people belonging to households with a monthly income of Rs 30,000 or less experienced discrimination from their neighbours or community due to being tested positive for the virus but only 7.3% from the highest income bracket faced similar issues. Additionally, 23.9% with an income of Rs 30,000 or less raised issues about the attitude of medical staff towards them, while those in the highest income bracket faced no such issues.
The National Health Profile in 2017 recorded one government allopathic doctor for every 10,189 people and one state-run hospital for every 90,343 people. India also ranks the lowest in the number of hospital beds per thousand population among the BRICS nations— Russia scores the highest (7.12), followed by China (4.3), South Africa (2.3), Brazil (2.1) and India (0.5). India also ranks lower than some of the lesser developed countries such as Bangladesh (0.87), Chile (2.11) and Mexico (0.98).
The report pointed out that the poor provisioning of public healthcare in India can be attributed to consistently low budget allocations. The current expenditure on health, by the centre and the state governments combined, is only about 1.25% of GDP, which is the lowest among the BRICS countries—Brazil (9.2%) has the highest allocation, followed by South Africa (8.1%), Russia (5.3%) and China (5%). It is also lower than some of its neighbouring countries such as Bhutan (2.5%) and Sri Lanka (1.6%).
The report made several recommendations to the Union government for improving the weak public healthcare system, existing health inequalities, and the ongoing pandemic. It said that the right to health should be enacted as a fundamental right that makes it obligatory for the government to ensure equal access to timely, acceptable, and affordable healthcare of appropriate quality and address the underlying determinants of health to close the gap in health outcomes between the rich and the poor.
It also said that the free vaccine policy should adopt an inclusive model to ensure that everyone, irrespective of their gender, caste, religion or location, that is people living in hard-to-reach areas, gets the vaccine without any delay. Further, regions with higher concentration of marginalised populations should be identified and public health facilities should be established, equipped and made fully functional as per the Indian Public Health Standard(IPHS).
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.
























