Why We Have Cows to Thank For the Eradication of Smallpox
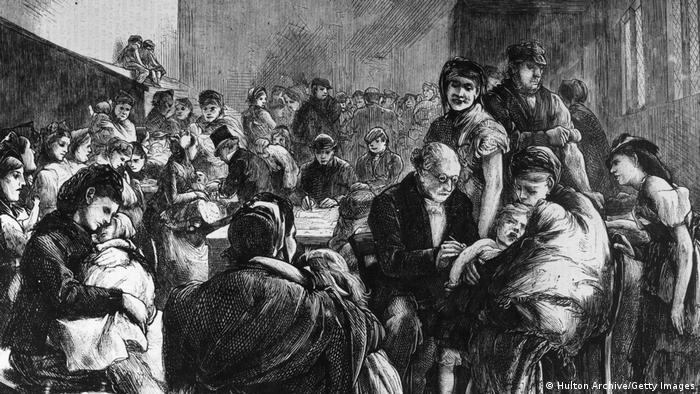
Smallpox inoculations were made freely available to people in many countries in the 19th Century.
May 8, 1980, marked the day of one of science’s greatest achievements: The eradication of the smallpox virus. Before that date, smallpox shaped the course of human history, killing untold millions around the world. In the 20th century alone, the virus claimed some 300 million lives.
After hundreds of years of intensive scientific and public health efforts, worldwide vaccination programs introduced in the 1970s put an end to the scourge of smallpox. But how was the world’s first vaccine developed, and why is it important that the vaccine is still stockpiled and utilized in cases of monkeypox?
Cowpox – learning from folk stories
The scientific origins of vaccines actually come from folklore. In the 18th century, it was rumored that milkmaids in England often caught mild cases of cowpox but rarely contracted smallpox.
Cowpox is a similar disease to smallpox, but milder and now known to be transmitted by a virus from the same family as smallpox.
When Dr. Edward Jenner, a physician, learned of these stories, he started experimenting with cowpox in his own work on inoculation. In the 1790s, Jenner used a needle to deliver a dose of cowpox pus under the skin of a 9-year-old boy. When the boy was later exposed to smallpox, he appeared to be immune.
Cowpox is a similar virus to smallpox, but symptoms are less severe
Jenner wasn’t the first to use pus to protect against infection. Similar procedures had already popped up independently in many regions of the world, including Turkey, China, Africa and India, as early as the 10th century. While Chinese doctors blew dried, ground-up smallpox material up the nose, Turkish and African doctors introduced pus under the skin, like Jenner. Although such methods were risky, people accepted a mild form of the disease and a low chance of death in exchange for protection from smallpox.
Despite its early origins, it wasn’t until Jenner’s research that the scientific and medical world took notice of the role pus could play in preventing smallpox. Jenner’s work created a proven and less risky method of protecting against smallpox, marking a turning point in treatment of the disease.
Inoculation spreads
Demand for inoculation spread around the world in the mid-late 19th century. In countries like England, Germany and the U.S., inoculation was free to all members of the public, and later made mandatory. High-society women were keen to receive inoculation to prevent a pockmarked face, while people inoculated or recovered from smallpox were permitted to work safely with children.
Inoculation programs were also driven by economic factors. Aristocratic classes understood smallpox outbreaks among the poor caused labor shortages. The case for free inoculation for everyone had as much to do with protecting individual health as with protecting societal wealth.
However, like today, inoculation programs were not universally celebrated. Many people saw the procedure’s small chance of death as being too risky, while religious objectors believed that inoculation interfered with God’s plans.
In the 19th century, anti-Semitic groups in Germany also claimed that vaccines were part of a global Jewish conspiracy to damage the German people. Similar anti-Semitic conspiracies were observed during the recent COVID-19 anti-vax movement.
A modern vaccine
The modern smallpox vaccine was created in the 1950s. More advanced scientific methods meant it could be isolated and freeze-dried to allow for long-term storage and stable distribution to sites around the world.
The new smallpox vaccine did not actually contain the smallpox virus, but vaccinia, a poxvirus similar to smallpox but less harmful. Like cowpox inoculations, vaccinia causes a small papule to develop in the skin, where the virus replicates. The body’s defense system then learns to recognize and destroy it.
Armed with this effective, safer method of fighting smallpox, the WHO launched its first major eradication campaign in the 1950s, with hopes to reach 80% vaccine coverage in each country.
The goal proved difficult, with vaccine supply and health infrastructure especially low in underdeveloped countries that lacked resources for public health programs of this scale.
Nevertheless, the program was highly successful. In 1966, smallpox remained endemic in just 33 countries. The very last illness caused by smallpox occurred in Somalia in 1977. Three years later, the WHO declared smallpox eradicated.

The development of modern vaccines brought safer and more effective protection against viruses
Smallpox vaccines still useful today
Eradicating smallpox is perhaps one of humanity’s greatest achievements. Smallpox was a particularly deadly disease, with fatality rates of around 30% for the variola major virus. Those who survived were often left with permanent scarring and had to overcome debilitating symptoms including fever, pain, exhaustion and vomiting.
Eradicating smallpox meant the world could breathe freely. But what can the world learn from this success?
The smallpox vaccination effort paved the way for multiple global vaccination programs, like that for polio and COVID-19. We owe the remarkable speed and effectiveness of the COVID-19 vaccination program to earlier smallpox efforts.
SARS-CoV-2, the virus that causes COVID-19, was first identified in December 2019, and the first vaccine was approved for use one year later in December 2020. Since then, global vaccination programs have been aiming to overcome issues with vaccine inequity to provide worldwide protection against the virus
Lastly, despite being eradicated, smallpox vaccinations are still useful today to help protect against similar viruses like monkeypox.
Currently, the smallpox virus Imvanex is approved in Germany for people who are at risk of contracting monkeypox, but it is not recommended for the general population as experts say it is unlikely that monkeypox will develop into a pandemic.
Edited by: Clare Roth
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.