Negative Thinking Could Be Risk Factor for Alzheimer’s Disease: Study
Image for representational use only.Image Courtesy : Psychology Today
How one’s mental state can influence biological processes is an emerging field of research and has got a new impetus in a study conducted on Alzhemier’s disease progression. Persistent negative thinking could raise the risk of progression of Alzheimer's disease, finds a new study by a team of University College of London (UCL).
The study was published in the journal Alzheimer’s and Dementia on June 7. The study was supported by the Alzheimer’s Society and took 292 participants in the age range of over 55 years that are part of the PREVENT-AD cohort study and also included 68 people from the IMAP+ cohort.
The study took responses of the participants over a period of two years to questions about their feeling of negative experiences, like ‘thinking deeply and worriedly about the past’ and ‘worrying more about the future’. The participants were also subjected to have completed measures of symptoms linked to depression and anxiety.
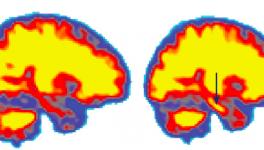
After their exposure to these questions, their cognitive functions were assessed by measuring memory, attention, cognitive ability of the spatial responses and also language. Out of them, 113 underwent brain scans using the PET (Positron Emission Tomography) scanning technique. The PET brain scans measured deposits of tau and amyloid, the two proteins that are hallmark of Alzheimer's. These two proteins aggregate in the brain and form tangles, which is believed to impair cognitive abilities of memories.
The brain scans and the repetitive negative thought responses led the researchers to discover an interesting correlation of negative thought pattern, declining cognitive abilities and the building up of amyloid and tau proteins in the brain. This, the study found, over a period of four years.
Natalie Marchant, the lead author of the study said about the findings: “Depression and anxiety in mid-life and old age are already known to be risk factors for dementia. Here, we found that certain thinking patterns implicated in depression and anxiety could be an underlying reason why people with those disorders are more likely to develop dementia. Taken alongside other studies, which link depression and anxiety with dementia risk, we expect that chronic negative thinking patterns over a long period of time could increase the risk of dementia. We do not think the evidence suggests that short-term setbacks would increase one's risk of dementia. We hope that our findings could be used to develop strategies to lower people's risk of dementia by helping them to reduce their negative thinking patterns.”
The findings uncover an important risk-assessing factor for the development of Alzheimer’s disease that could turn the memory ability of a patient upside down. Further, new ways of early prevention can also be brought about, like providing new ways of mental training practices to the elderly who fall prey to repetitive negative thinking patterns. For example, talk therapy which can help someone come out of a negative thought spree. Regarding this, Gael Chetalat, a co-author of the study, said: “Looking after your mental health is important, and it should be a major public health priority, as it's not only important for people's health and well-being in the short term, but it could also impact your eventual risk of dementia.”
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.