Effective Communication Can Undo Fear, Phobia and Anti-Vaccine Prejudice—Dr K Srinath Reddy

Noted cardiologist and epidemiologist Dr K Srinath Reddy is president of the Public Health Foundation of India and author of Make Health in India: Reaching a Billion Plus. In an interview with Rashme Sehgal, he talks about mutations in the Novel Coronavirus, how mass vaccination is the key to control the Covid-19 pandemic and that “fear, phobia and prejudice of anti-vaccine campaigners” needs to be checked by communicating accurate information on vaccine development and rollout. Edited excerpts:
How justified are apprehensions of the virus mutating? And if that is indeed the case, how effective will the vaccines against Covid-19 prove?
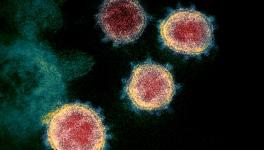
There can be minor mutations and major mutations, which may variably alter infectivity and virulence. However, some of the viral components being targeted by the vaccines are unlikely to be altered by these mutations. Especially, the “Spike Protein” which is the most frequently targeted viral component. That is what the virus uses to gain entry into the cell and also gives it the name “Corona”. So, mutations are unlikely to make the vaccines ineffective as long as the virus does not shed its spiky crown.
What do think about the new strain of the Novel Coronavirus, which has emerged in the United Kingdom and mainland Europe?
The new strain is reported to be about 70% more infectious. However, it has not increased its virulence. Even so, if the number of people getting infected increases and the fraction of persons getting very sick or dying remains the same, the absolute number of people getting very sick or dying will rise. That will put pressure on our health system and pose danger to vulnerable persons. We must do our best to prevent the entry and spread of this strain in our country.
Some leading virologists have expressed reservations about the mRNA Covid-19 vaccines. For example, Dr Gifty Immanuel has said that the mRNA is a highly fragile molecule that must be stored at minus 70 degrees and this was a failure against influenza. Your comments?
The potential effects of a vaccine may be assessed by a study of the biological pathways of action; and the actual effects through clinical trials of efficacy and safety. The first is done through animal studies. Following such experimental research, which is examined by a regulator, clinical trials in humans are permitted to be undertaken in three phases. At each stage, regulatory agencies evaluate safety data before giving permission to proceed further. In the case of the mRNA vaccines, all of these stages have been completed. If the regulatory agencies have done their job well, there is no reason to believe that they have overlooked evidence of serious harm or lack of efficacy. The regulatory process in the USA also involves a public hearing.
We have no reason, at this stage, to believe that the vaccines are ineffective. Safety issues will continue to be studied even after the vaccine begins to get administered to the general population, after the regulatory approval. This post-licensure surveillance is called a phase 4 study. If serious adverse effects are observed at this stage, the approval for the vaccine can be cancelled. At present, there is no evidence to suggest that the vaccines have bypassed strict regulatory scrutiny of either the animal studies or the clinical trials. Besides the mRNA vaccines, there are other vaccines under trial with different platforms such as virus vector and inactivated virus platforms. They too are being evaluated for safety and efficacy through the same stepwise assessment.
The mRNA is indeed a fragile molecule. Hence it is coated with a fatty layer (lipid nanoparticles) to protect it till it is transported into the cell. While the Pfizer BioNTech vaccine demands a minus 70-degrees Celsius temperature, the Moderna vaccine requires minus 20-degrees temperature for storage. Such cold-chain requirements are challenging for a large-scale vaccination programme. India will have to look for other vaccines, as will many other countries.
Several doctors have questioned the amazing vaccine matrices coming out which show 98% to 100% efficacy. There are also some questions about how long vaccine-induced immunity will last. Is there a concern that we are rushing through with these vaccines?
The claims have ranged from 90-95% for some vaccines and 62% for one dosing schedule of the Oxford vaccine. Before the trials began, international regulatory agencies and the WHO had set a success criterion of 50% efficacy, with a lower confidence limit of 30% for any observed point estimate. The reported results far exceed those, for the primary endpoint of symptomatic Covid-19. The lower confidence limit, in statistical terms, would be lower than 90%. However, even that lower limit of the confidence band would be much higher than 50% in these large trials.
We do not know how long the immunity lasts. Based on both antibody levels as well as T-cell immunity studies in persons with the natural infection, the acquired adaptive immunity may last up to six months. Since this is a new virus, data from natural infections does not provide more insights at this time. Vaccines may produce longer lasting immunity, than the natural infection, due to the standardised dose of the antigenic stimulus and the booster second dose. However, we still need to study the duration of protection. The toll the pandemic has taken on health, education, economy and social life globally is a reason why vaccines are being taken up avidly, even if we are uncertain about the duration of protection.
You have said that a key way to know the efficacy of the [Novel] Coronavirus is by finding out how many people demonstrate infection from the immunised and the non-immunised group. Are the details of this still under study?
Every phase 3 vaccine trial has a group which is vaccinated with the active vaccine and a comparison group which gets a placebo. These are randomly allocated across the trial participants. The rates of occurrence of a pre-determined outcome are compared between the two groups when the trial is completed. That is being done even in these vaccine trials. The pre-determined endpoint is “symptomatic Covid-19” and not infection per se. The intent of these vaccines, administered by the intramuscular route, is to prevent illness [disease] due to the virus even if they cannot stop the initial entry of the virus [infection]. For the latter, we may need “sterilising” mucosal vaccines, which are inhaled. They are still in early stages of evaluation.
How effective will a vaccine be for those who have compromised immune systems?
Persons may be immunocompromised due to diseases that lower immunity or severe malnutrition, or immunosuppressed (due to treatments for some diseases). There are two challenges in such situations. Is the vaccine safe? Is it effective?
Live attenuated vaccines, virus-vector vaccines and DNA vaccines will have safety concerns in such cases. While mRNA vaccines may be safe, but we have no proof of that from the trials, as such persons were not included. On theoretical considerations, inactivated virus vaccines are likely to be the safest in such persons.
The vaccines may be unable to generate adequate levels of protective immunity in persons with compromised or therapeutically suppressed immune systems. In such persons, early administration of specific monoclonal or polyclonal antibodies, after exposure to any active Covid-19 case will help in combating the virus, through passive immunity.
We do not know the long-term effects of these vaccines and some patients developed reactions when they were administered with a vaccine. Is fear one of the main reasons why an anti-vaccine movement has developed in the West?
Uncertainty about the safety and efficacy of vaccines exists in many minds. Fear, phobia and prejudice of anti-vaccine campaigners feed on the uncertainty of even those who are not blindly opposed to vaccines, to create hesitancy and even rejection. It is important to have open debates [and] clear communication on what is known and unknown, as well regular updating of evidence-based recommendations.
The fact that reactions occurred in a few persons who received the vaccine was widely publicised. That is good, as open disclosure is ethically needed. Some of them were persons with known allergic disorders. So, caution has now been sounded for such persons. However, the vast majority of persons appear to have received and tolerated their first dose well. We will get better information after more persons receive the second dose too. Persons who have doubts can wait longer to see how others are faring in their own country after receiving the vaccine.
For long-term effects, we will still have to gather data for some months to come (phase 4 surveillance). Some persons have proposed that phase 3 trials should continue even if efficacy has been shown and regulatory approval has been given, to assess long term safety as well as differential response in sub-groups. Others question the ethical soundness of such an approach, once an effective vaccine is available.
To be vaccinating a sizeable adult section of the population in India will prove a huge challenge. Adar Poonawalla of the Serum Institute in Pune has repeatedly said it will take up to 2024 for the vaccine to reach every Indian. Is that the aim of a vaccine—to reach all?
We do not know if the vaccine conferred immunity lasts for several years. That seems unlikely. So, we do not know how many of those vaccinated early will need to be revaccinated. It is also likely that we may have more vaccines available next year, which are manufactured in India and get our regulatory approval. So, it is speculative to put a calendar year on the time of “complete” vaccine rollout in India.
Herd immunity is a concept which says that if an X% of people in a population gets immunity (through natural infection or vaccination) they will block the transmission of the virus and thereby protect the Y% in the population who are uninfected or unvaccinated from infection. We still do not know what that herd immunity threshold (X%) is, for this virus. Also, if an unvaccinated non-immune person (from the Y group) travels to another location where the population immunity levels are well below X%, that Y person is no longer protected by the protective cordon offered by the first herd. So, while herd immunity may work at the population level, it is best for each person to get immunity at the individual level. Especially, if they wish to travel within or outside the country.
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.