Unholy Nexus Trumps Public Health

Medicines can save lives and ameliorate suffering. In the past decades, medicines have contributed enormously to improvements in population health as people across the world, in spite of unacceptable inequities, are generally healthier than before and live longer. But medicines can also kill people and cause disease and suffering. Diseases caused by the adverse effects of medicines are called iatrogenic diseases and typically can account for 20% of hospital admissions. The lay public is generally ignorant of this aspect of the use of medicines, believing naively that more medicines mean better health. This is a view that has been fostered by the pharmaceutical industry, which project medicines as the answer to all forms of human suffering.
Companies are interested in selling larger and larger quantities of medicines as they stand to make more profits if more medicines are consumed. While pushing for increased medicines consumption, the companies invariably gloss over the fact that all medicines have side effects that are harmful. We use medicines while knowing that they can cause harm because the benefits are likely to be much larger than the possible risks. When drug regulators allow medicines to be manufactured and marketed they balance the possible benefits against risks and only allow those medicines where the benefits are much larger than risks due to side effects. Drug regulators may also decide to withdraw old medicines when new medicines become available, which treat the same condition but have fewer adverse effects.
Thus all medicines are poisons, but we consciously use them, doctors prescribe them, and regulators allow them to be marketed because their potential benefits can be enormous – outweighing the possible adverse effects. If we understand that medicines can also harm our health, it would be clear that the aim should be to treat a disease with the lowest number of medicines that can effectively treat the disease. By being conscious about the need to use fewer medicines, we seek to minimise the possibility of adverse effects. When you buy a medicine you can see that the package insert mentions tens to hundreds of possible side effects. These adverse effects are usually seen in a very small percentage of people, so the possibility of a person being harmed by a prescribed medicine is usually very low. But if we consume several medicines at the same time, the chances that at least one of them will cause harmful effects starts rising.
Fixed Dose Drug Combinations should be exceptions
The above is the central reason why it is usually not a good idea to combine two or more medicines in the same formulation – tablet, syrup, injection, etc. When we do combine two or more medicines in a single formulation they are called ‘Fixed Dose Combinations (FDCs),’ so named as the ingredients are present in a fixed ratio.
For prescribers and patients, FDCs appear to offer an attractive option as it is easier to take a single FDC rather than two or more medicines at the same time. But there are only a very small percentage of patients who need to take more than one drug for the same disease. Also medicines differ from each other in the way they act in the body. Some may stay in the body for long; some may be flushed out of the body within a few hours. Some medicines are absorbed better before food, some after meals. When FDCs are used, it becomes impossible to vary the dose and scheduling of individual medicines. Experience across the world also shows that if FDCs are available easily, doctors tend to prescribe them even when a single ingredient drug would suffice. In addition to multiplying the possibility of adverse effects, the use of FDCs also increases the cost of treatment.
There are, however, some indications for the prescription and use of FDCs. Some diseases such as TB, HIV and some forms of malaria need to be treated with more than one drug. In these diseases, treating with a single drug may actually be harmful as this increases the possibility of the pathogen (bacteria or virus) developing resistance to the drug used.
There are also some drugs that, when used together, reinforce their individual effects – so the effect of the FDC is more than the sum of the effects of the drugs that are combined together. Thus, in the anti-micobrial drug, Co-trimaxozole, Trimethoprim potentiates the action of the Sulpha drug it is combined with. Similarly Clauvulanic acid potentiates the action of Amoxycillin in an FDC that combines the two. These are exceptions and not the rule, and that is why the World Health Organisaton’s list of essential medicines and the Indian Essential Medicines list contain less than 30 FDCs out of a total of 400 drugs.
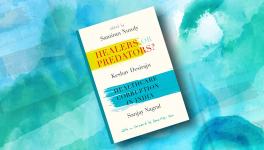
Indian Market Choked by Irrational FDCs
The situation in India is dramatically different. There are thousands of FDCs (real estimates are not available) and 30,000 or more brands of these FDCs. Overall, estimates suggest that a quarter to half of drugs in the Indian market are FDCs. Such a situation contributes enormously to irrational use of medicines, increase in treatment cost and leads to multiplication of side effects of treatment. Medicines, instead of contributing to better health, are, as a result, contributing to diseases caused by excessive and unscientific intake of unnecessary medicines. It is in this context that we need to understand the recent Gazette notification by the Government, banning 328 FDCs.
The new notification is another episode in a long list of blundering steps taken by the government in the past decades. The fact that the Indian market is flooded with irrational FDCs, the fact that it is unscientific to prescribe most FDCs, the fact that companies willingly flout laws to manufacture and market irrational FDCs, and the fact that the Government has been singularly unwilling to implement the law of the land, are widely acknowledged. Why, then, does this practice continue to be rampant? Underlying this situation is a corrupt nexus involving a section of drug companies, unscrupulous or ignorant doctors and corrupt drug regulators. The 59th Report of the Standing Committee on Health and Family Welfare, on ‘The Functioning of the Central Drug Standard Control Organisation (CDSCO)’, released in 2012, has documented evidence of this nexus in detail.
Laws Flouted With Impunity
Since 1961, laws have existed in India that require scientific scrutiny of all FDCs before they are allowed to be sold. Companies, hand in glove with corrupt regulators, utilised some ambiguity in the law to fraudulently obtain approval from state-level regulators. The law was tightened in 1988 but the practice continued, with full knowledge of the central drug regulatory agency. Given growing demands from public health practitioners and public interest organisations, the CDSCO, in 2007, signaled its intention to ban 294 FDCs. In practice, these were never banned! Several meetings of expert committees followed and in 2016, the Government issued a notification banning 344 FDCs. Companies promptly approached the courts and the order was stayed by the Delhi High Court.
The challenge of the ban order by drug companies, including by some of the largest MNCs like Pfizer, Glaxosmithkline and Abbott, was a disingenuous attempt by them to preserve their profits and to profiteer at the expense of public health. Most of the FDCs banned were not even registered in countries with strong regulatory systems. Further, as these drugs have no therapeutic validity, their sales are driven by unethical marketing practices of drug companies, such as financial and other inducements offered to prescribers.
The Delhi High Court, gave in to the arguments of high-profile lawyers hired by drug companies, and did not even consider the technical issues related to the ban. The stay order was pronounced on a technicality, that the Drug Technical Advisory Board (DTAB), had not been consulted before the ban order. It took two years for the government to get the DTAB to meet and uphold the scientific validity of the ban order. Base on this the Gazette notification banning 328 FDCs was issued in September 2018.
Companies have again rushed to various courts challenging the ban and courts have stayed the imposition of the ban in the case of some drugs, based on the plea that they were registered before 1988 (when, as we note earlier, the ambiguity in law was removed).
Conclusions
Several issues stand out and need to be emphasised. First, the ban covers a measly 300 odd drugs while there are thousands of bogus FDCs in the market (which translates into over 20,000 brands of different companies). Industry estimates are that only 2-3% of the market is affected by the ban while estimates indicate that at least a quarter (some say almost half) of the Indian market consists of irrational FDCs.
Second, the saga of the government continuing to drag its feet on an urgent public health issues, continues. Successive governments have taken decades to respond with real measures and even today the ban order covers a fraction of the irrational FDC market.
Third, is the misuse of the judicial system in India. It is a matter of deep concern that some of the top MNCs are trying to defend the continued marketing of so-called cough syrups such as Phensedyl and Corex, which are actually being consumed as addictive substances as they contain the opiate called Codeine. In 2017, the Narcotics Control Bureau (NCB) had asked the Drug Controller General of India (DCGI) to “substantially reduce” the availability of codeine-based cough syrups and tramadol preparations (which provide pain relief for post-surgery pain and cancer treatment), saying they are being used as narcotic drugs. The NCB routinely seizes huge consignments of these drugs while being smuggled to neighbouring countries. Clearly the government needs to do a far better job in informing courts about the hazards posed by some drugs, and courts, too, need to balance public interest with commercial interests.
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.