Why North-East Is India’s Worst Cancer Afflicted Region
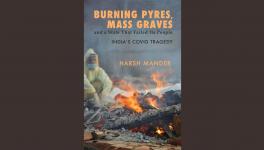
Representational use only.
Guwahati: Farhan Ali’s husband, in his late 70s, was unable to gulp any water as the cancer growing out of his stomach spread to his mouth through his throat. Earlier, being a muezzin in his village, Kalgachia, meant her husband was used to summoning his followers for daily prayers. “Even villagers from nearby Goalpara and Bilasipara villages would gather to hear his soulful azaan,” Farhan recalled.
A 113-km round trip to Guwahati costs them around Rs 3,500 a day. After a year-long chase of three doctors, stretching their finances over Rs 4,00,000, the family finally landed in the Dr B Borooah Cancer Institute (BBCI), the busiest and oldest full-fledged cancer care facility in the Northeast. “At the last hospital, the doctor apprised us of cancer. Looking over our household income, we were referred here. Else, the treatment would be over Rs 9,000,00,” Farhan said. Seated at a waiting room in BBCI since 5:30 AM, she reserves the next chair with a loaded school bag; her husband and kin queuing in front of a Surgical Oncology department.
The National Cancer Registry Programme Report (NCRP), 2020, recorded the highest incidence of cancers in Northeastern India between 2012 and 2016. Nasopharynx, stomach, hypopharynx, oesophagus, liver, gallbladder, larynx, lung, breast and cervix uteri were the common cancer types, the report read. The estimated cancer burden in Aizawl district in Mizoram and Papumpare in Arunachal Pradesh was the highest: 269.4 and 219.8 among men and women respectively, per lakh population. Trailing the adjoining states were Meghalaya’s East Khasi Hills—227.9 cases per lakh and Assam’s Kamrup (urban)—213 cases per lakh.
A region battered by exceptional rates of cancer– doctors claim states such as Meghalaya, Nagaland and Mizoram rank no. 1 in the world for certain cancers–has patients from remote villages hustling hundreds of kilometres in difficult hilly terrains, across shifting sandbar islands and arcane living root bridges for basic cancer treatment. Given the lack of oncologists, cancer treating hospitals, and specialised infrastructure there are forlorn hopes of potentially life-saving treatment.
Pathetic Cancer Care Infrastructure
The hallmark of most comprehensive cancer centres (CCC) involves the delivery of surgery, radiation, chemotherapy and palliative care to the afflicted patients. However, barely one-fifth of the districts in the region are served by the CCCs. There are: six CCCs in two districts of Assam, one CCC in one district of Arunachal Pradesh, two CCCs in two districts of Manipur, two CCCs in one district of Nagaland , one CCC in one district of Mizoram; one CCC in one district of Meghalaya, and one CCC in one district of Tripura.
Also read: COVID-19 Looms Over North-East, But is it Prepared?
With no access to reliable data on the number of oncologists in the region, NewsClick gathered a rough estimate through its correspondence with experts. Taking off from the sole CCCs in some states, there are only two radiation oncologists at Sikkim’s Sir Thutob Namgyal Memorial Hospital in Gangtok, three at Arunachal Pradesh’s Tomo Riba Institute of Health and Medical Sciences (TRIHMS), and seven at Tripura’s Regional Cancer Centre. According to Dr C Tetseo, State Nodal Officer at the NTCP (National Tobacco Control Programme), Nagaland, “There are only 2-3 oncologists in the entire region of Nagaland.”
Raising concerns on the density of oncologists in the North Eastern region(NER), Dr Dhaneshwar Naorem, an oncologist at Manipur’s Babina Specialty Hospital said, “The total number of oncologists is not even half of what is required to level the high cancer incidence. Relatively, Assam has ample oncologists but the distribution is uneven, only limited to specific districts.”
Back in the BBCI, inside the OPD Building, two rows of black-upholstered chairs stacked against each other are always packed. Among the seat-holders, some sprawl out in the space of two-three chairs. As afternoon glides towards evening, weary-eyed parents rest on their children’s laps, biding their time.
Outside Dr. Gaurav Das’s Surgical Oncology OPD, a teenage boy on a wheel-chair covers a jutting bone in his leg with a plain handkerchief. For the boy, Gaurav Das suggested, "Cancer on his fibula bone can be treated without removing the affected leg through the bone tumour surgery only available at the BBCI."
Also read: Grim Picture of NRHM: Ailing CHCs and Shortage of Doctors
Bondona Sonowal (name changed), draped in a light blue mekhela chador, underwent two botched surgeries, over Rs 1,00,000, in Dibrugarh for her breast cancer. As she was sifting rice by hand, a push against a breast lump, led to her suspicion. “The first doctor cut too much off my breast. The bleeding wouldn’t stop. I had to get a stitch from another doctor to stop bleeding,” she recalled.
Even for breast cancer, the BBCI is the preferred choice for surgeries sparing the breast, added Gaurav Das. Bondona’s treatment, costing over Rs. 60,000, was provided free-of-charge under Assam’s government’s Atal-Amrit Abhiyan scheme, whose maximum limit is Rs. 2 lakh p.a. for an individual member.
The penetration of radiation equipment across the NER is low: Mizoram, Arunachal, Sikkim have one radiotherapy machine at their only state-run cancer-treating hospitals. In most cases, the cancer welfare schemes, though present, are availed by the low-income patients only when they have been pushed to the edge of poverty after tirelessly changing referrals.
In places where Primary Health Cares (PHCs) are the nominal first point of referrals, a group of regional volunteers have banded together to form an NGO, to guide cancer patients from remote villages to lone tertiary cancer care centres in their state. For instance, during one of their yearly visits to Dasi, Anini and Seppa villages to raise awareness about high-tobacco consumption and cancer, members of the Arunachal Cancer Welfare Society picked up six-year-old Pisu Cheda from Seppa, 200 kms from Itanagar.
By the time, Pisu Cheda reached AP’s lone cancer centre i.e. TRIHMS, she was diagnosed with aplastic anemia, a rare condition where the body stops producing new blood cells. Living through unemployment, her family couldn’t afford her treatment. The treatment for child cancer care, which is usually advised in a specialised paediatric cancer unit is only available at cancer hospitals in Guwahati.
“We raised around Rs. 1,40,000 through crowd-funding over two months, and another Rs 10,000 by collaborating with AMG Accessories, which sold jewellery to collect funds for further treatment in Guwahati,” said Bomnya Kombak, member secretary of the Arunachal Cancer Welfare Society. With the setting of lockdown that enforced state-border closures, and nowhere else to turn to, the doctors at the TRIHMS, Naharlagun (a part of Itanagar Capital Complex), fought the absence of resources to administer cancer care for her, covered under the Chief Minister’s Free Cancer Therapy, whose maximum ceiling is Rs. 10 lakh per patient per year.
In faraway Punjab, representatives of the Tata Memorial Centre have been operating a hub at Mullanpur near Chandipur and a spoke in Sangrur, to pull the state out of its worst cancer crisis. Almost 8,000 patients avail highly subsidised treatment at the Sangrur spoke annually. A Parliamentary Committee Report evinced interest in the replication of the model – where the BBCI would be developed as a hub for the North Eastern states with “immediate focus on infrastructure development and training of human resources at all levels, until similar hubs and spokes are set up in all North Eastern states”.
Now, as an integral of TMC, the BBCI is expected to be a hub catering to 4 crore population, which is the approximate population of NE India, alongside peripheral smaller cancer treatment facilities (spokes) catering to 40 to 50 lakh population, said Manigreeva Krishnatreya, medical officer cum in-charge at BBCI. “The need for massive resources for the creation of spokes can be meted out through the inclusion of BBCI’s administrative support and oncology trainees,” he pointed out.
High Tobacco Consumption Levels: A Cancer Nightmare
Leaning forward on his seat at the BBCI waiting room, Shobigul Islam, a resident of Goroimari village, fiddles with his cellphone. As he presses back to catch a break, he narrated how his 60-year-old father’s habitual smoking turned to a nightmare. “My father stopped smoking as he spat blood. When medicines costing over Rs 4,000 couldn’t provide relief, we turned to a local quack for help but to no avail.”
Cancers related to tobacco are not uncommon, rather the highest in the NER, said the NCRP 2020 report. A Global Adult Tobacco Survey, 2016-17,(GATS2), shows Tripura, Mizoram, Manipur, Assam, Meghalaya, Arunachal Pradesh and Nagaland posting percentages over 40 – outranking the other states for the consumption of tobacco in any form. “The challenges to the efficacy of tobacco control drives are the socially acceptable practices of tobacco consumption, like paan tamul (betel and areca nut) in Assam, or tuibur (tobacco water) in Mizoram,” points out Arundhati Deka, State Nodal Officer, NTCP, Assam.
Also read: Covid-19: Terminally Ill Patients Stare at Unfolding Catastrophe Amid Lockdown
Mizoram, the state with a record 34.4% for smoking–the highest in the country–has been grappling with the influx of cheap Chinese cigarettes across its porous border with Myanmar and Bangladesh. On July 1, 2015, the Hindu Business Line reported sights of ‘a pack of 20 Chinese FarStar cigarettes priced at Rs 40 ’ and ‘a pack of 20 Winbody at Rs. 25’ along the area from Aizawl to Champai. Attractively packed, sold at half the cost of an Indian Flake, they are easily accessible to youths and customers in lower-income groups–making tobacco control an uphill task.
R. Lalremruata, a state consultant at the Mizoram Tobacco Control Cell, told NewsClick, “ A shift towards Chinese cigarettes from the ITC-branded ones has been observed among the people of Mizoram for economical reasons. After the State ban on foreign cigarettes, I cannot say these cigarettes are not available but they are not advertised in full view,” adding, “Some merchants who approached us to get permits for repackaging such cigarettes were not allowed.”
Alongside cigarettes, the highest prevalence of smokeless tobacco use in Tripura, Manipur, Assam, Arunachal Pradesh and Nagaland in GATS2 survey has set the alarm bells ringing for tobacco cessation. State Tobacco Control Cells have been up their neck in influencing the tobacco use trends.
For example, in Mizoram, a smoker caught in a public place has the option of reimbursing 50% of the fine if he decides to quit smoking, thereby registering at the State Tobacco Cessation Clinic, explained R. Lalremruata, Mizoram NTCP State Consultant.
In Tripura, drop boxes have been specifically designed for patients or their kins to toss their tobacco products away before entering any medical institution, said Moutoushi Deb, State consultant at NTCP (Tripura). Although state-wide clampdowns on cigarettes and other tobacco products have intensified, Dr C Tetseo marked drily, “Reining in current trends of smokeless tobacco use among youths, which is strikingly high, is untenable under the provisions of the present law.”
Is Cancer The Price to Pay For Cherished Ethnic Delicacies?
The report compiled by the NCRP 2020 mentions “local cultural factors and lifestyle choices'' as factors contributing to the differences in cancer incidence pattern in India, “as was seen in Thailand.” Dr. Vikas Jagtap, a radiation oncologist at the North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences (NEIGHRIMS), Shillong attributes Meghalaya’s high incidence of oesophagus cancer to avidly consumed locally brewed drinks, paan (betel leaf) relished with slaked lime and areca nut, and smoked and fermented meat.
Sam Tsering, Arunachal Pradesh’s Nodal Officer for Cancer Control Programme reckons 45% of the 700-1000 patients he visits at the TRIHMS every year are diagnosed with stomach cancer linked to mostly genetic and dietary factors instead of tobacco use. “Even the liver cancer incidence rates are on account of lack of awareness about Hepatitis-B infections'', he explained.
Also read: Will NITI Aayog’s Proposed PPP Model Make District Hospitals Inaccessible for the Needy?
The practice of consumption of traditional varieties of smoked and fermented meat, mostly common in the NER, shares similarities to the avidly consumed fermented cyprinoid fishes, the source of high prevalence of bile duct cancer in Northeastern Thailand. As a matter of fact, the battle against deeply ingrained love for sour and fermented fishes since generations was won by Thailand’s Ministry of Public Health advocating the use of cooked fish and cleanliness practices that spared liver flukes causing bile duct cancer. The allopathic treatment of cancer shrugs off the individual lifestyle management of a patient, an often alleged cause to cancer occurrences.
Integrated Cancer Care
Integrated cancer care at Akesis Life, an immuno oncology centre in Bangkok–one-way of bringing remission to cancer-afflicted patients– combines drugs and surgeries with traditional Chinese medicines, homeopathy, nutrition and mental well-being, improving the efficacy of cancer treatments.
Dr. Sasithorn Sachdev, a practitioner of integrated cancer care at Akesis Life recalled the effects of integrated cancer care on a patient suffering from Hodkin’s lymphoma in his centre. Initially, he subsisted on a mix of ethnic and western diet which was replaced with a wholesome plant-based diet complemented with juice and water fasting during chemotherapy.
“He was able to retain remission during our ongoing full integrative programme for 12 weeks. There were minimal side effects of chemotherapy seen in his case. The mental health experts helped him counter mounting stress, enabling him to cope with his condition,” he added. After the completion of the program, the patient would receive a diet-maintenance plan focusing on the change in his lifestyle. “The difference is we are treating the person, not the disease,” Dr Sachdev said.
Two years ago, Bengaluru-based oncology startup, Carer, was founded to extend the benefits of personalised integrated cancer treatment to its patients. It’s owner, Samara Mahindra told NewClick, “No amount of cancer care in India is comprehensive without the combination of allopathic treatments with lifestyle management, which means integrated cancer care. Cancer is most likely to recur if you ignore a patient’s lifestyle.”
However, waging a blame game on flagrant lifestyle choices erases bigger problems at play, to the point of perpetuating stereotypical assumptions and misrepresenting one’s own experience of cancer, according to Gaurav Pramanik (35), a social activist from North Bengal and Sikkim, who is also a cancer survivor. “You can blame a thousand things, such as smoked pork, akhuni or kinema (fermented soybean), tongba (local millet wine) but you cannot discount the fact that we already live in a carcinogenic world,” he emphasised.
(The author is a freelance journalist based in Northeast India. Views are personal)
Get the latest reports & analysis with people's perspective on Protests, movements & deep analytical videos, discussions of the current affairs in your Telegram app. Subscribe to NewsClick's Telegram channel & get Real-Time updates on stories, as they get published on our website.